Help Transform Recovery1‑3


Help give continuous protection from opioid‑rewarding effects all month after the first dose1
A single injection of SUBLOCADE® was sufficient to completely block the rewarding effects of hydromorphone, a higher-potency opioid, in most participants when measured 1 week post‑injection1,4
- Has a higher binding affinity than most other opioids6,7*
- Has an analgesic potency approximately 2‑8x greater than morphine4
- Has a rapid onset of action (the analgesic action of hydromorphone is perceived within 15 minutes following intramuscular injection)4,8
- May be abused via injection, similarly to heroin4
*Binding affinity is an in vitro measurement and may not correlate with clinical potency.7
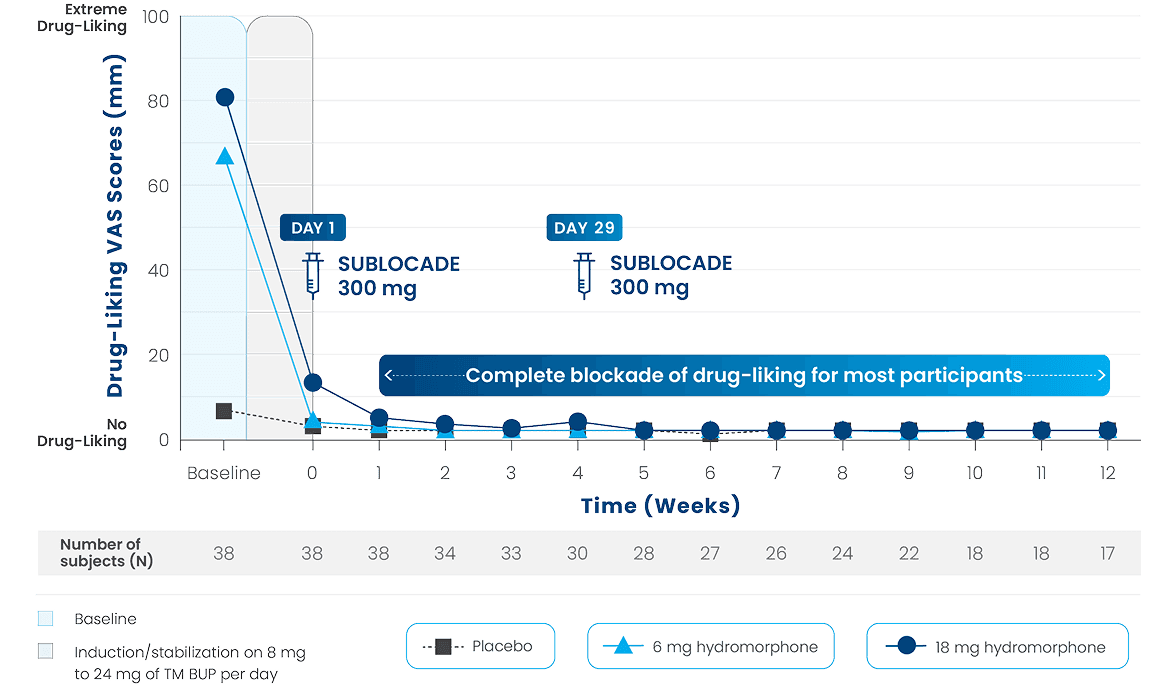
The figure shows median peak (Emax) drug-liking VAS scores (ranging from no drug-liking to extreme drug-liking) over 12 weeks for participants receiving SUBLOCADE 300 mg (on Day 1 and Day 29) following weekly challenges with placebo, hydromorphone 6 mg, or hydromorphone 18 mg, in a randomized order. The horizontal line at 20 mm delineates the noninferiority margin for opioid blockade. Beneath that treatment week indicator is the number of subjects (N) who provided those VAS measurements for all 3 challenges with placebo, hydromorphone 6 mg, and hydromorphone 18 mg.1,5
The figure shows median peak (Emax) drug-liking VAS scores (ranging from no drug-liking to extreme drug-liking) over 12 weeks for participants receiving SUBLOCADE 300 mg (on Day 1 and Day 29) following weekly challenges with placebo, hydromorphone 6 mg, or hydromorphone 18 mg, in a randomized order. The horizontal line at 20 mm delineates the noninferiority margin for opioid blockade. Beneath that treatment week indicator is the number of subjects (N) who provided those VAS measurements for all 3 challenges with placebo, hydromorphone 6 mg, and hydromorphone 18 mg.1,5
TM BUP=transmucosal buprenorphine; VAS=visual analog scale.
(13-0002, NCT02044094)1
In this 12-week study, non‑treatment-seeking participants with OUD received 300 mg of SUBLOCADE on Day 1 (n=39) and Day 29 (n=30). Participants were challenged with both doses of hydromorphone (6‑mg and 18‑mg) or placebo (1) at baseline, (2) at the end of the induction/stabilization period of TM BUP, and (3) during each of the 12 weeks of the study for 3 consecutive days (each week on Days 5‑7) in a randomized fashion.1,5
- Prior to the first injection of SUBLOCADE, participants started with a required induction and dose-stabilization period with TM BUP. Induction occurred over 3 days and dose-stabilization over a period of 4 to 11 days. Though not seeking treatment, 77% (30/39) of participants returned for the second dose of SUBLOCADE
The study was not designed or intended to draw any head-to-head comparisons between TM BUP and SUBLOCADE.5
Primary objective: Demonstrate that the peak (Emax) effect of drug-liking for 6 mg and 18 mg intramuscular hydromorphone challenges following subcutaneous injections of SUBLOCADE 300 mg was noninferior (ie, hydromorphone was not substantially more likable) to the peak effect of drug-liking of the placebo challenge as measured by a unipolar 100‑point VAS.1,5
PK assessments: Buprenorphine plasma levels were taken (1) immediately before each hydromorphone challenge, (2) before and 1.5 hours after TM BUP, and (3) before and 24 hours after each SUBLOCADE injection.5,9
Select Inclusion criteria for participants10
Participants needed to meet DSM-5 criteria for moderate or severe OUD at screening and not be seeking treatment for OUD
- Aged 18-55 years
- BMI 18-33.0 kg/m2
- Current or historical experience with parenteral abuse of opioids
- Experiencing signs and symptoms of withdrawal prior to the start of buprenorphine‑naloxone sublingual film dosing (as evidenced by a COWS score >12)
- Women of childbearing potential (defined as all women who are not surgically sterile or postmenopausal for ≥1 year prior to informed consent) must have a negative pregnancy test prior to enrollment and must agree to use a medically acceptable means of contraception from screening through ≥3 months after the last dose of study drug
- Male subjects with female partners of childbearing potential must agree to use medically acceptable contraception from screening through ≥3 months after the last dose of study drug
- Normal or no clinically significant ECG findings at screening
- Total bilirubin ≤1.5 × ULN, ALT ≤3 × ULN, AST ≤3 × ULN, serum creatinine ≤2 × ULN, INR ≤1.5 × ULN
ALT=alanine transaminase; AST=aspartate aminotransferase; BMI=body mass index; COWS=clinical opiate withdrawal scale; DSM-5=Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; ECG=electrocardiogram; INR=international normalized ratio; OUD=opioid use disorder; PK=pharmacokinetic; TM BUP=transmucosal buprenorphine; ULN=upper limit of normal; VAS=visual analog scale.
INDICATION
SUBLOCADE, with counseling and psychosocial support, is for moderate to severe opioid use disorder in those who have initiated treatment with a dose of transmucosal buprenorphine or are being treated with buprenorphine.
IMPORTANT SAFETY INFORMATION
WARNING: RISK OF SERIOUS HARM OR DEATH WITH INTRAVENOUS ADMINISTRATION; SUBLOCADE RISK EVALUATION AND MITIGATION STRATEGY
- Serious harm or death could result if administered intravenously. SUBLOCADE forms a solid mass upon contact with body fluids and may cause occlusion, local tissue damage, and thrombo-embolic events, including life threatening pulmonary emboli, if administered intravenously.
- Because of the risk of serious harm or death that could result from intravenous self-administration, SUBLOCADE is only available through a restricted program called the SUBLOCADE REMS Program. Healthcare settings and pharmacies that order and dispense SUBLOCADE must be certified in this program and comply with the REMS requirements.
CONTRAINDICATIONS: SUBLOCADE should not be administered to patients who are hypersensitive to buprenorphine or any component of the delivery system.
WARNINGS AND PRECAUTIONS
Addiction, Abuse, and Misuse: SUBLOCADE contains buprenorphine, a Schedule III controlled substance that can be abused in a manner similar to other opioids. Buprenorphine is sought by people with opioid use disorder and is subject to criminal diversion. Monitor patients for conditions indicative of diversion or progression of opioid dependence and addictive behaviors.
Risk of Life-Threatening Respiratory Depression and Concomitant Use of Benzodiazepines or Other CNS Depressants with Buprenorphine: Buprenorphine has been associated with life-threatening respiratory depression, overdose, and death, particularly when misused by self-injection or with concomitant use of benzodiazepines or other CNS depressants, including alcohol. Warn patients of the potential danger of self-administration of benzodiazepines, other CNS depressants, opioid analgesics, and alcohol while under treatment with SUBLOCADE. Counsel patients that such medications should not be used concomitantly unless supervised by a healthcare provider.
Use with caution in patients with compromised respiratory function (e.g., chronic obstructive pulmonary disease, cor pulmonale, decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression).
Opioids can cause sleep-related breathing disorders, e.g., central sleep apnea (CSA), sleep-related hypoxemia. Opioid use increases the risk of CSA in a dose-dependent fashion. Consider decreasing the opioid using best practices for opioid taper if CSA occurs.
Strongly consider prescribing naloxone at the time SUBLOCADE is initiated or renewed because patients being treated for opioid use disorder have the potential for relapse, putting them at risk for opioid overdose. Educate patients and caregivers on how to recognize respiratory depression and, if naloxone is prescribed, how to treat with naloxone. Emphasize the importance of calling 911 or getting emergency help, even if naloxone is administered.
Risk of Serious Injection Site Reactions: The most common injection site reactions are pain, erythema and pruritus with some involving abscess, ulceration, and necrosis. Some cases resulted in surgical depot removal, debridement, antibiotic administration, and SUBLOCADE discontinuation. The likelihood of serious injection site reactions may increase with inadvertent intramuscular or intradermal administration. Carefully review injection technique.
Neonatal Opioid Withdrawal Syndrome: Neonatal opioid withdrawal syndrome (NOWS) is an expected and treatable outcome of prolonged use of opioids during pregnancy. NOWS may be life-threatening if not recognized and treated in the neonate. Newborns should be observed for signs of NOWS and managed accordingly. Advise pregnant women receiving opioid addiction treatment with SUBLOCADE of the risk of neonatal opioid withdrawal syndrome.
Adrenal Insufficiency: Adrenal insufficiency has been reported with opioid use. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off the opioid.
Discontinuation of SUBLOCADE Treatment: Due to the long-acting nature of SUBLOCADE, if treatment is discontinued, monitor patients for several months for withdrawal and treat appropriately.
Inform patients that they may have detectable levels of buprenorphine for a prolonged period of time after treatment with SUBLOCADE. Considerations of drug-drug interactions, buprenorphine effects, and analgesia may continue to be relevant for several months after the last injection.
Risk of Hepatitis, Hepatic Events: Because cases of cytolytic hepatitis and hepatitis with jaundice have been observed in individuals receiving buprenorphine, monitor liver function tests prior to treatment and monthly during treatment.
Hypersensitivity Reactions: Hypersensitivity to buprenorphine-containing products have been reported most commonly as rashes, hives, and pruritus. Some cases of bronchospasm, angioneurotic edema, and anaphylactic shock have also been reported.
Precipitation of Opioid Withdrawal in Patients Dependent on Full Agonist Opioids: Buprenorphine may precipitate opioid withdrawal signs and symptoms in persons who are currently physically dependent on full opioid agonists if administered before the effects have subsided, at least 6 hours for short-acting opioids and 24 hours for long-acting opioids. Verify that patients have tolerated transmucosal buprenorphine before administering the first injection of SUBLOCADE.
Risks Associated With Treatment of Emergent Acute Pain: When patients need acute pain management, or may require anesthesia, treat patients receiving SUBLOCADE currently or within the last 6 months with a non-opioid analgesic whenever possible. If opioid therapy is required, patients may be treated with a high-affinity full opioid analgesic under the supervision of a physician, with particular attention to respiratory function, as higher doses may be required for analgesic effect and therefore, a higher potential for toxicity exists with opioid administration.
Advise patients of the importance of instructing their family members, in the event of emergency, to inform the treating healthcare provider or emergency room staff that the patient is physically dependent on an opioid and that the patient is being treated with SUBLOCADE.
Use in Opioid Naïve Patients: Because death has been reported for opioid naïve individuals who received buprenorphine sublingual tablet, SUBLOCADE is not appropriate for use in opioid naïve patients.
Use in Patients With Impaired Hepatic Function: Because buprenorphine levels cannot be rapidly decreased, SUBLOCADE is not recommended for patients with pre-existing moderate to severe hepatic impairment. Patients who develop moderate to severe hepatic impairment while being treated with SUBLOCADE should be monitored for several months for signs and symptoms of toxicity or overdose caused by increased levels of buprenorphine.
QTc Prolongation: QT studies with buprenorphine products have demonstrated QT prolongation ≤ 15 msec. Buprenorphine is unlikely to be pro-arrhythmic when used alone in patients without risk factors. The risk of combining buprenorphine with other QT-prolonging agents is not known. Consider these observations when prescribing SUBLOCADE to patients with risk factors such as hypokalemia, bradycardia, recent conversion from atrial fibrillation, congestive heart failure, digitalis therapy, baseline QT prolongation, subclinical long-QT syndrome, or severe hypomagnesemia.
Impairment of Ability to Drive or Operate Machinery: SUBLOCADE may impair the mental or physical abilities required for the performance of potentially dangerous tasks such as driving a car or operating machinery. Caution patients about driving or operating hazardous machinery until they are reasonably certain that SUBLOCADE does not adversely affect their ability to engage in such activities.
Orthostatic Hypotension: Buprenorphine may produce orthostatic hypotension.
Elevation of Cerebrospinal Fluid Pressure: Buprenorphine may elevate cerebrospinal fluid pressure and should be used with caution in patients with head injury, intracranial lesions, and other circumstances when cerebrospinal pressure may be increased. Buprenorphine can produce miosis and changes in the level of consciousness that may interfere with patient evaluation.
Elevation of Intracholedochal Pressure: Buprenorphine has been shown to increase intracholedochal pressure, as do other opioids, and thus should be administered with caution to patients with dysfunction of the biliary tract.
Effects in Acute Abdominal Conditions: Buprenorphine may obscure the diagnosis or clinical course of patients with acute abdominal conditions.
Unintentional Pediatric Exposure: Buprenorphine can cause severe, possibly fatal, respiratory depression in children who are accidentally exposed to it.
ADVERSE REACTIONS: Adverse reactions commonly associated with SUBLOCADE (≥5% of subjects) during clinical trials were constipation, headache, nausea, vomiting, increased hepatic enzymes, fatigue, and injection site pain and pruritus. This is not a complete list of potential adverse events. Please see the full Prescribing Information for a complete list.
DRUG INTERACTIONS
CYP3A4 Inhibitors and Inducers: Monitor patients starting or ending CYP3A4 inhibitors or inducers for potential over- or under-dosing.
Serotonergic Drugs: If concomitant use with serotonergic drugs is warranted, monitor for serotonin syndrome, particularly during treatment initiation, and during dose adjustment of the serotonergic drug.
Consult the full Prescribing Information for SUBLOCADE for more information on potentially significant drug interactions.
USE IN SPECIFIC POPULATIONS
Pregnancy: Opioid-dependent women on buprenorphine maintenance therapy may require additional analgesia during labor.
Lactation: Buprenorphine passes into the mother's milk. Advise breastfeeding women to monitor the infant for increased drowsiness and breathing difficulties.
Fertility: Chronic use of opioids may cause reduced fertility. It is not known whether these effects on fertility are reversible.
Geriatric Patients: Monitor geriatric patients receiving SUBLOCADE for sedation or respiratory depression.
To report a pregnancy or side effects associated with taking SUBLOCADE or any safety related information, product complaint, request for medical information, or product query, please contact PatientSafetyNA@indivior.com or 1-877-782-6966.
See full Prescribing Information, including Boxed Warning, and Medication Guide. For REMS information visit www.sublocadeREMS.com.
P-BAG-US-01758 April 2025